Our Experts Track Every Claim Using a Simplified Approach for Effective Aging AR Recovery
We drill down to the root cause for which the claim was denied.
The identified reasons are then categorized and assigned to respective teams for corrective action.
Upon receiving the claims from respective departments, they are resubmitted for a claim.
Tracking the status of the resubmitted claims with regular follow-ups.
Preparing a handy checklist of top denial reasons and how to handle them.
Creating a second-level check based on the findings of the denial reasons to avoid future rejections.
At Medstream RCM, we empower our clients to get paid faster. Specifically, we achieve this by delivering effective denial management solutions that resolve denied and rejected claims while addressing their root causes. Furthermore, our dedicated team actively investigates and reviews all denials to resolve issues and resubmit insurance claims efficiently. In addition to that, we systematically identify and tackle problems to ensure you receive your payments on time.
Moreover, we offer comprehensive medical billing and revenue cycle management services that are tailored for clinicians, practices, and hospitals. Therefore, you can trust us to optimize your revenue cycle and streamline your payment processes.
Medstream RCM offers a robust and comprehensive medical billing solution that guarantees meticulous attention to detail. We proactively follow up on every claim submitted to the insurance company, diligently tracking each one until it is fully processed and resolved. Regardless of whether the claim is large or small, our A/R Follow-Up services utilize a systematic approach to ensure that nothing falls through the cracks. Consequently, we strive to maximize your practice’s reimbursement potential for the services rendered. By integrating our focused efforts with your needs, we aim to deliver the highest level of financial return possible.
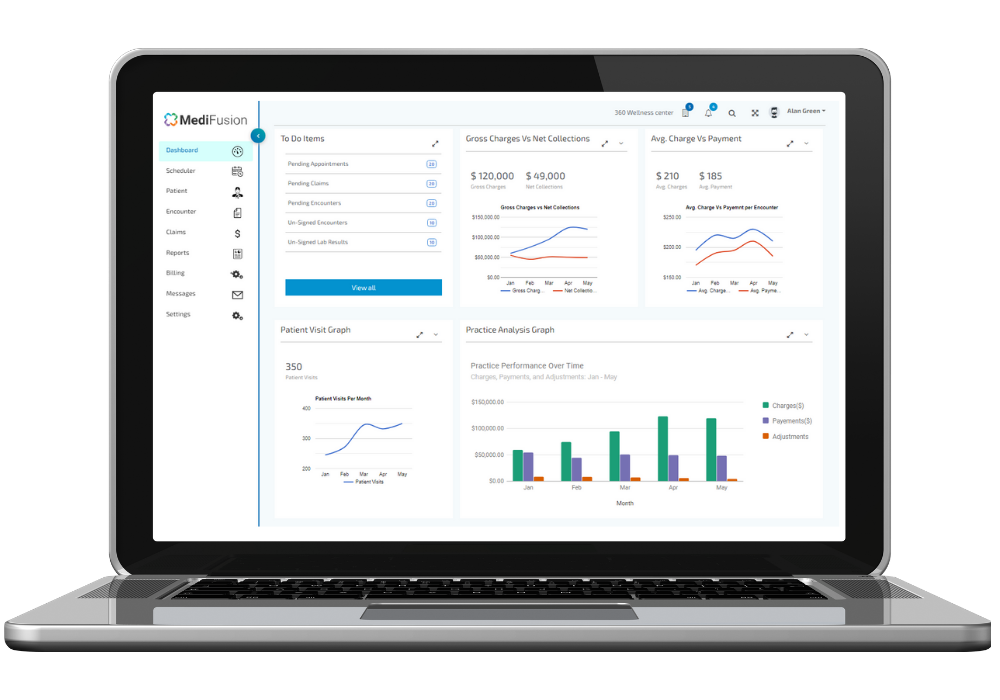
Our Denial Management team actively boosts your payment recovery by identifying the root causes of denied claims and equipping you with the necessary tools for timely resolution. With our integrated suite of software, MediFusion, we automatically route denied claims to the appropriate staff members for immediate follow-up and systematic corrections.
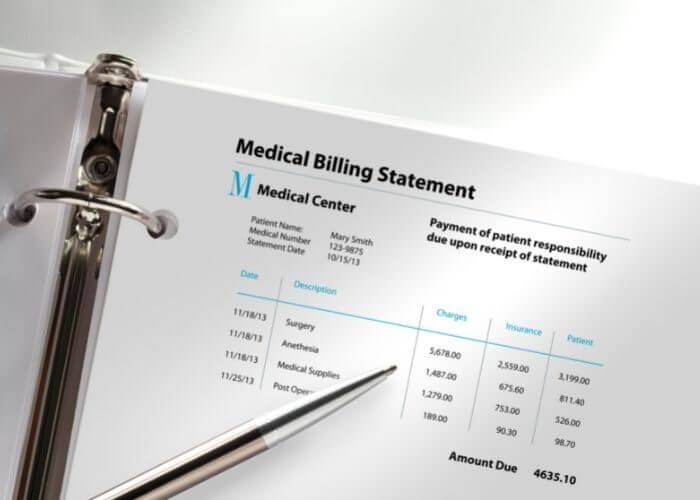
Medstream RCM empowers you to submit error-free claims, analyze rejected claims, and track down denials and non-payments. Our top-tier Medical Billing AR services actively include:
– Improving provider documentation and enhancing data reporting.
– Conducting thorough in-network and out-of-network AR follow-up.
– Following up on Workers’ Compensation claims.
– Negotiating directly with claims adjusters.
– Sending out various levels of appeals when claims are not paid.
– Engaging in proactive patient AR follow-up.
– Cleaning up and auditing credit balances.
– Managing old accounts receivable effectively.


Subscribe your Email address for latest news & updates