We Handle the Paperwork, So You Can Focus on Patient Care
At Medstream RCM, our team maintains expertise in the provider credentialing process. We stay updated on industry changes and trends. As experts, we manage the credentialing process from start to finish. Our team handles responsibilities that typically fall on your staff. This allows your team to focus on more important tasks.
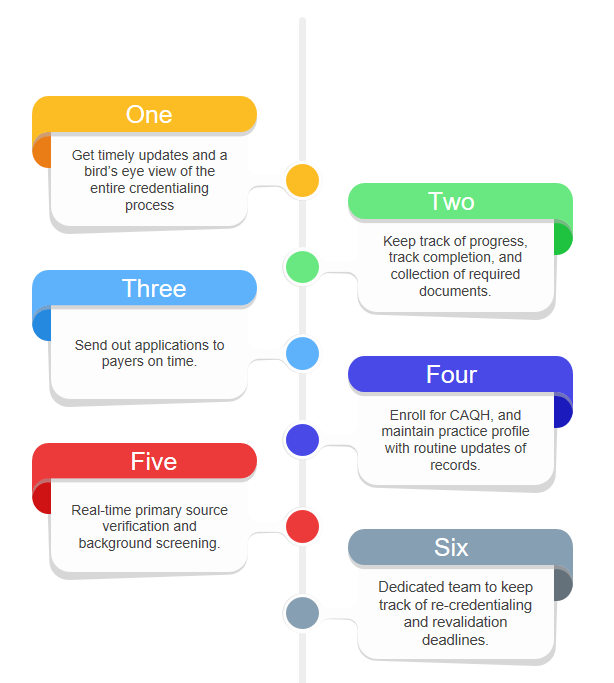
We track document completion and gather necessary information. Our experts complete the credentialing process and send applications to payers. We swiftly respond to requests for corrections or additional information. At Medstream RCM, we monitor re-credentialing deadlines for your practice. We initiate and complete the process when due.
Our team collaborates with providers to fill out initial applications. We perform tasks required by the organization, including primary source verification. We also conduct background screening and coordinate with payers. This ensures timely approval and expedites provider starts.
Trust the experts at Medstream RCM to help you navigate the difficult process of provider enrollment and medical credentialing, all at a low cost! No more cash flow problems & not being paid. No more data errors. No more accidental expirations, we’ll end all your headaches. Contact us today.
We help your practice gather the necessary background and demographics information.
We help providers enroll for CAQH and also assist them with profile maintenance and updating of records.
Ensure the preparation of all necessary documentation required before submitting the applications to the payers.
Manage all follow-up activities and tasks such as verification and communication with the payer organizations.
Get complete access to our Electronic Health Records and credentialing system, as you can always view everything we're doing without having to wonder what's going on.
We provide a dedicated account manager who is an easy sole point of contact and knows everything about the credentialing for your medical organization.
Provider credentialing is essential for medical practices. Services that cannot be billed are not sustainable. The credentialing process ensures providers meet required standards. It also identifies risk factors early on. This early identification helps reduce adverse outcomes. Credentialing improves public relations and attracts new patients. It helps in gaining patient trust. Although time-consuming, credentialing protects revenues. It limits potential losses and enhances practice reputation.
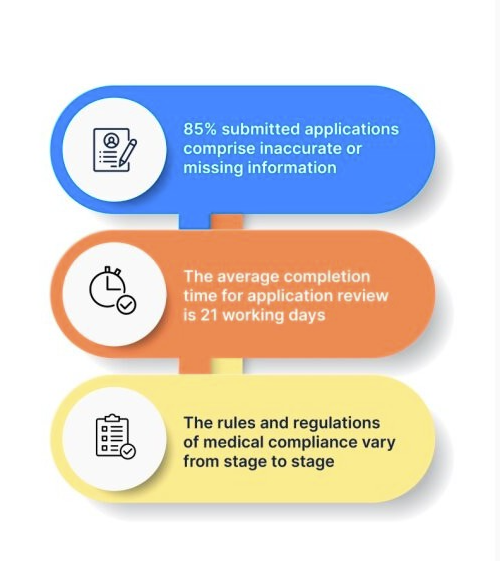
Many practitioners try to manage the medical provider credentialing process in-house. However, after reviewing the expenses, most find outsourcing to Medstream RCM is more cost-effective.
When you outsource credentialing to a professional team, your efforts can be streamlined. While your staff might credential one or two providers, our team can handle dozens every day. This not only saves money but also valuable time for your staff.
Your team can then focus on more important tasks, ensuring the growth of your practice. Let our Credentialing Service take care of provider credentialing and ongoing maintenance.
Our experts understand payers, their needs, and the necessary actions for successful credentialing. Medstream RCM provides monthly updates and complete transparency throughout the payer credentialing process.


Subscribe your Email address for latest news & updates